Medication Storage in Care Homes

Estimated Reading Time: 6 minutes
When it comes to storing medicines safely in care homes, care home providers have a wide range of information that they must provide for the staff (registered nurses and social care practitioners) in the form of a written policy.
From storage conditions to self-administered medicines, there's a lot to think about.
Kickstart your care search
Discover the best care homes in your area through Lottie.
How and Where to Store Medicines
Care home providers must state how and where to store medicines, including:
- Medicines supplied in monitored dosage systems and original packaging
- Controlled drugs - when it comes to storing controlled drugs, care home providers must follow the Misuse of Drugs Regulations
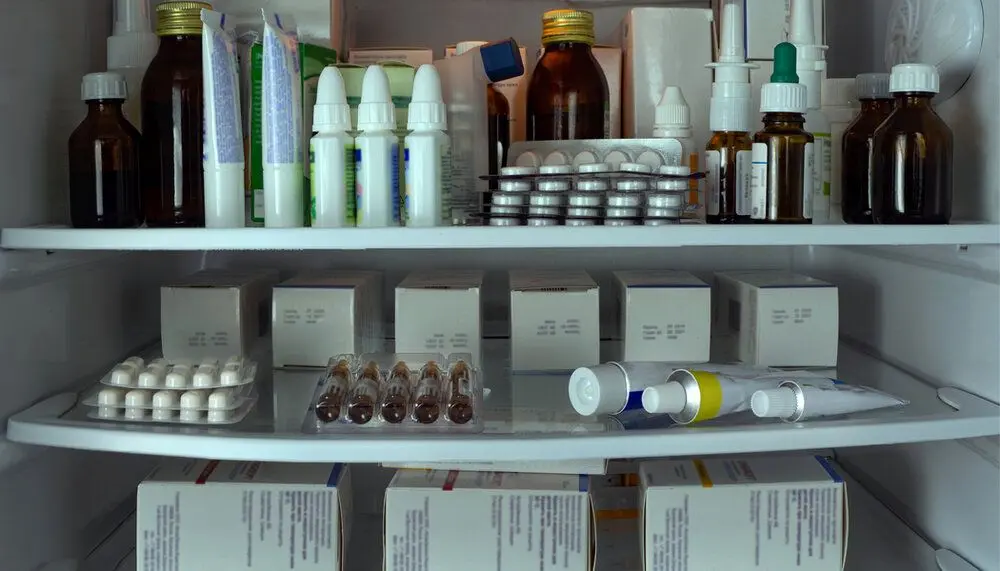
- Medicines that need to be stored in a refrigerator
- Skin creams and other topical preparations
- Nutritional supplements and thickeners
- Appliances and devices, including sharps
Care home providers must provide secure storage conditions with only authorised care home staff having access and they must provide the conditions that medication requires to be stored. And each resident’s medicine may require different storage conditions, these storage conditions must meet the needs of the resident, choices, risk assessment and type of medicine system they are using.
Temperatures
Care homes are recommended to take the same approach and advice that applies to pharmacies in England.
Care home providers must create policies and processes that address the temperature requirements for storing different medicines. These processes must include how the care home staff should monitor the storage conditions in order to ensure they are stored according to the manufacturer’s recommendations.
Each provider's policy should guide care home staff to take daily temperature readings and use an air conditioner or storage cooler if needed.
Refrigerated Medicines
Most kinds of medicines come with directions stating to store them below 30C or 25C. This is due to the fact that some medicines actually begin to break down and degrade after they are manufactured.
For the majority of medicines, this process can take years, but they can become less active over time.
In order to satisfy the National Institute for Health and Care Excellence’s (NICE) guidelines on managing medicines in care homes, keeping temperature records to show they have been monitored and controlled is sufficient.
Storage Conditions
It must be taken into consideration that different medicines may require different storage conditions however, good practice is to store medication:
- Away from heat, dampness and light sources
- Some medication may require being stored in a refrigerator
- In a place where a certain resident’s medication can not be mixed up with others
- In a secure storage place where it could not be stolen
- Where they do not pose a risk to anyone
- In hygienic conditions
- Within their expiry and use by date
In residential care homes, medicines can be stored by individuals in their own rooms or centrally by the care home staff, however in the case of residents storing and handling their own medication, risk assessments must be carried out to ensure the safety of everyone involved.
Secure Storage
Medicines must be stored securely in care homes. Only authorised care home staff should be able to access the medicine, a care home’s policy must state how to ensure the keys are securely stored.
Self-administered medicines
Self-administration is when an individual can take their own medicines. As stated by the Care Quality Commission, “people have the right to choose and manage their own medicines and staff should consider a person’s choice and whether there is a risk to them or others.
According to NICE, care home staff should assume that a resident can take and look after their own medicines themselves (self-administer) unless a risk assessment has indicated otherwise. These risk assessments must be taken out by health and social care practitioners in order to find out the level of support each resident needs to carry on taking and storing their medicines themselves.
Dosette boxes make it easier for residents to manage their own medication routine.
This risk assessment should consider:
- Resident’s choice
- If self-administration would be a risk to themselves or others
- If the resident can take the correct dose of their own medicine at the correct time and in the right way
- How often the risk assessment should be carried out
- How the medicines will be stored
These risk assessments should be done individually for each resident (and their family members or carers if the resident wishes) by care home staff with the correct training and skills.
Based on this risk assessment, the responsibilities of the care home staff and the location and security of the resident’s medicine should be written down in the resident’s individual care plan.
People should also be able to access any medicines they need when they need to take or use them. It’s also vital that no other residents have access to these medicines.
Emergency Medicines
In the case of emergency medicines being required, they must be stored so that care home staff can access them quickly. In case an emergency happens where a resident requires medication, there must always be sufficient adequately trained staff (at least one on every shift, day and night) to administer the medication and assist during an emergency.
Disposal
Before care home staff dispose of a medicine, they should look to see whether it is still needed, if the medicine is within its expiry date and the shelf-life if it has been opened.
There should be records of all medicines that have been disposed of at all times, and medicines that are waiting to be disposed of should be kept in a locked and tamper-proof place until they are collected or taken to the pharmacy.
When disposing of medicines or clinical waste, care home providers should have a process for the quick disposal of medicines that exceed requirements, unwanted medicines (including those of residents who have passed away) and any expired medicines.
Lottie matches care seekers with the best care homes for their needs. You can request a free care home shortlist from our care experts, who will share homes matching your budget, location and type of care needed. You can also search for a care home through our easy-to-use directory.



